Antimicrobial resistance
AMR is an urgent global health threat.
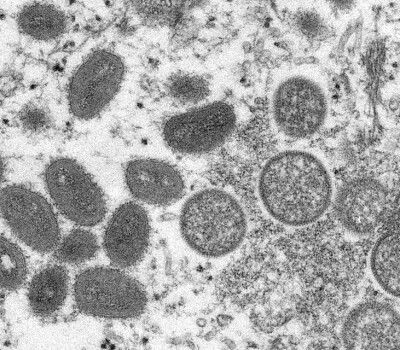
Antimicrobial resistance (AMR) develops when bacteria, viruses, fungi and parasites change over time and no longer respond to treatment. Globalisation, migration and (medical) tourism will inevitably lead to the worldwide spread of new (multi-)resistant mutant pathogens.
Resistance to antibiotics is a problem across many different domains. The ecological, sanitary and socioeconomic conditions that promote the propagation of antibiotics have never disappeared. Due to urbanisation, population growth and migration, the situation has even deteriorated in many areas.
Units

Monitoring appropriate use of antibiotics
It is of great urgency to change how patients are diagnosed and how antibiotics are prescribed, distributed and used. In addition, the role of animal health care and infection prevention and control in health care facilities cannot be ignored. Adequate diagnostic and treatment facilities are scarce. To make matters worse, antibiotics of uncontrolled, often inadequate quality are widely available to uninformed populations and unlicensed or unskilled health providers. Untreatable infections become alarmingly frequent, while the research and development pipeline in the pharmacological industry is extremely thin.

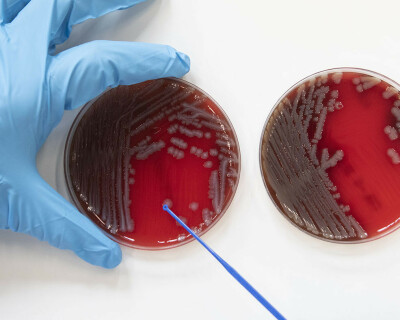
What we do
ITM is coordinating research projects to combat antibiotic resistance. An interdisciplinary approach is required to counter this persistent threat. Scientists of the institute collaborate on novel diagnostic tools and treatment strategies for infection prevention and control, promote responsible antibiotic use, and investigate human, social and cultural factors.